WARNING: This post contains material of a sensitive and sexual nature. If you are easily embarrassed or squeamish, you might want to sit this one out.
I saw the Urology Department Physician Assistant the week after my surgery to take out my catheter. She gave me a prescription for 50mg sildenafil (generic Viagra) tablets and told me to take a half tablet every night “to keep the blood flowing” – a prophylactic Roto-Rooter®. I made an appointment with her and the Vacuum Erection Device Clinic for January as “the December clinic had already passed.” I was supposed to talk with the clinic about acquiring a “medically approved” vacuum erection device in January, but I pushed to get it ordered in December since they run upwards of three hundred bucks and I’d met my deductible for the year.
I got a mysterious text message from FedEx alerting me to a delivery from upcrx.com that required my signature. Often “signature required” means either someone is sending alcohol, or the IRS wants to do an audit. Google helped me find University Compounding Pharmacy in San Diego but did nothing to alleviate my confusion.
The package arrived the following week. I scrawled my name on the driver’s tablet and I now possessed my very own prescription “Austin Powers Swedish Penis Enlarger.” I wasn’t supposed to use it until after my postoperative appointment in January, and then only “under medical supervision,” lest I somehow injure myself.
I had an appointment in January with Dr. Fine for a postoperative visit. The PSA level I’d had drawn the previous week was undetectable; I’d get a PSA level done every three months for a year, then every six months if all went well.
He asked about my recovery.
“It’s going fine. The big incision burned every time I moved but that went away in a week and I used the Norco maybe three times. I got by on Tylenol. And I’m back to my pre-surgical level of incontinence.”
His eyes lit up!
“You should really see one of the pelvic physical therapists. There are a couple of people who specialize in male incontinence therapy.”
“I’m fine.”
“You really should consider it; nip it in the bud right now.”
(Like I have the time or inclination to have some dude teach me Kegel exercises, which I’d taught women for decades.)
“Ok, I’ll give them a call.” (No, I won’t.)
Many physicians are hardwired to offer as many labs, procedures, and referrals as possible. That is probably why sleep studies have been such a standard for anyone who is fat, diabetic, hypertensive, and/or chronically tired. He gave me the phone number which I tossed into the trash on my way to the car.
It’s been seven months since surgery; I don’t wear underwear shields anymore and the urgency is almost nonexistent. I may not be able to write my name in the snow but it no longer feels like I’m trying to urinate through a urethra in a death grip.
The following week I saw the P.A. She had asked me to come in early because she had to go somewhere. Today she was a little frantic and hurried through her instructions.
“You’ll be talking to Jonathan about the vacuum. Stop taking the Viagra while you are using it. Try the Viagra after a couple of weeks. If you don’t see any results after several tries, it’s time to open this little white bag and take the pill that’s in there. If you’re still not getting any results after 2 months, you need to come see me. Here’s an instruction sheet. Now I have to go…”
My next stop was the pretentiously named Vacuum Erection Device Clinic. I figured I’d be in a classroom with several other men discussing our surgical recovery, led by a physician in the requisite white coat giving us a talk on the mechanism of tumescence and how our recent surgery had interfered with function.
Instead, I went to another room and met with the “physician liaison” (read: equipment rep).
“I’ll need to order your device and when it comes in, we can talk about how to use it.”
“Uh, I got it last month.”
“Ok, then. Here’s what you do. Put it over your penis. Pump the vacuum for five or ten seconds, then wait forty-five seconds. Release the vacuum, wait a minute, and then pump it again for five to ten seconds and wait forty-five seconds. Do that for 10 minutes a day. If you have any questions, here’s my card.”
I wasted an afternoon for this?
How an erection works.
The cross-section of the penis looks like a cartoon monkey face. The shaft of the penis contains two spongy cylinders, the corpus cavernosum; a sizeable artery runs through each. A vein flanked on each side by an artery and a nerve runs above the corpus cavernosum. All this is surrounded by a layer of fascia, like a hot dog casing. A third spongy tube, the corpus spongiosum, surrounds the urethra and runs the length of the shaft below the corpus cavernosum while the dorsal penile vein runs the length of the shaft on top. All this is enclosed in loose tissue and covered by thin, flexible skin.
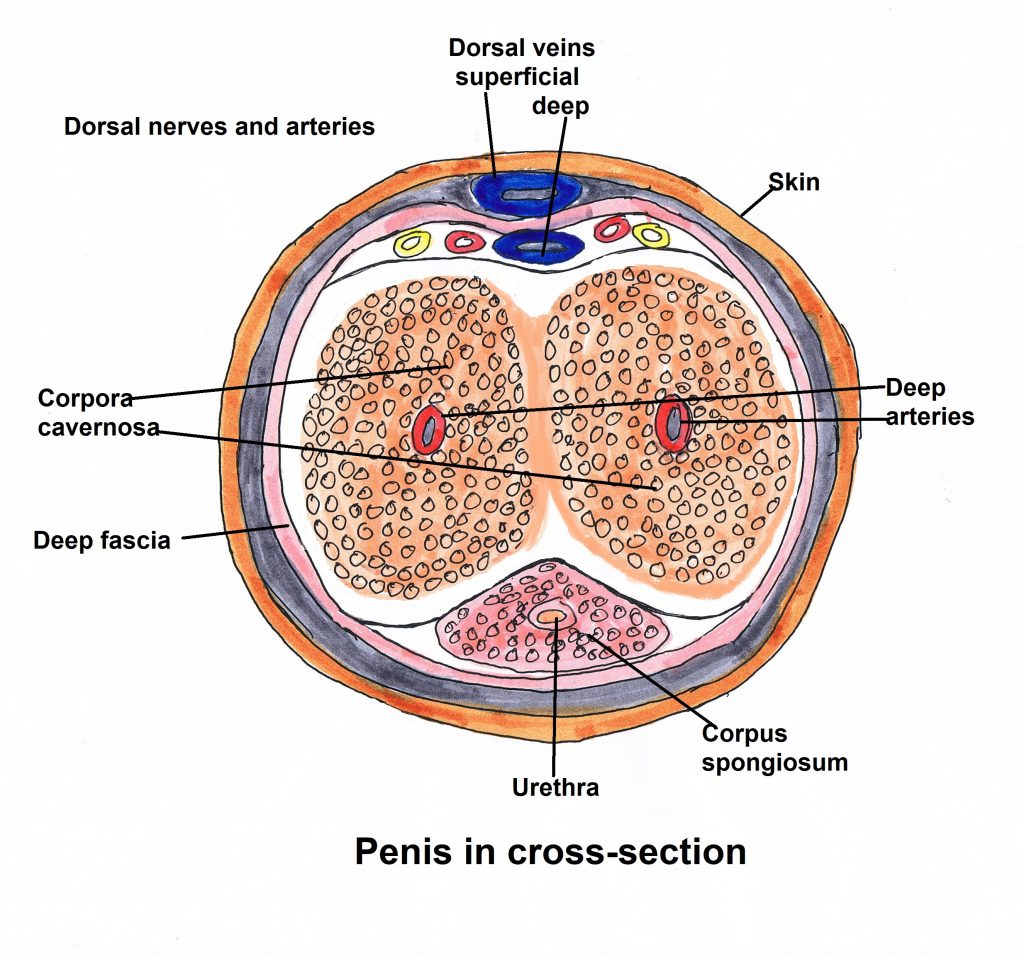
The arteries in the corpus cavernosum normally aren’t fully open, which is why men don’t have permanent erections. When the brain is stimulated, a combination of nerve impulses and chemical signals open the arteries which fill the corpus cavernosum with blood. The engorged tissue presses on the veins, blocking return blood flow and, voilà, an erection is born.
It’s been suggested that men hit their sexual peaks at 18 and it’s downhill after that. Research, however, shows men’s testosterone levels peak in their 30s before gradually declining. Getting an embarrassing, spontaneous erection for no apparent reason disappeared by my late teens. Sexual function can decline as early as one’s 40s; I started noticing a difference in my late 40s. Other things can affect sexual drive and function besides purely aging:
- medical conditions (diabetes, high blood pressure, heart disease, obesity, depression)
- certain medications (blood pressure medications, antidepressants, narcotics and others)
- Bad habits (excessive alcohol consumption, smoking, recreational drugs, lack of sleep)
- neurological disorders (Parkinson’s, multiple sclerosis, spinal cord lesions)
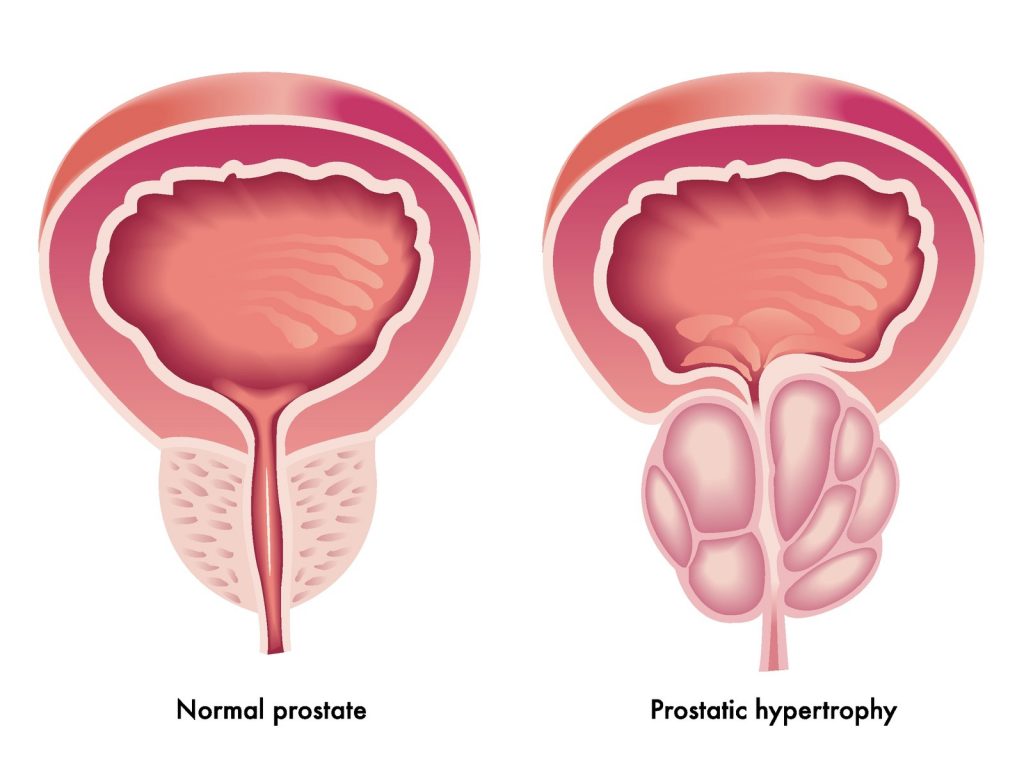
- an enlarged prostate or, in my case
- treatment for prostate cancer
The nerve bundles required for achieving an erection are often damaged during a radical prostatectomy. Scarring around my prostate required taking out the neurovascular bundle on the right side. The left side was spared but the trauma from surgery is enough to keep the remaining nerves from doing their job. It may take up to two years before being able to achieve an erection with or without ED drugs. If that doesn’t work, the alternatives are injections into the penis or penile implants.
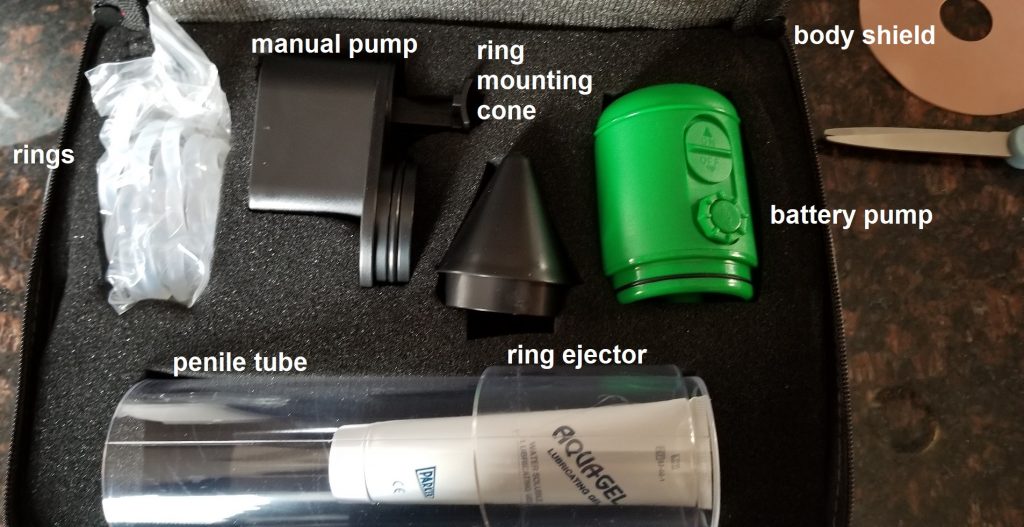
This is my device. It has both battery-operated and manual vacuum pumps which attach to an acrylic cylinder. There are five silicone rings (sizes 5 to 9); the cone is used to slip a ring onto the other end of the cylinder. The ring ejector twists to push the ring onto the penis before removing the cylinder to maintain the erection. The body shield is that circular thing resembling a old-fashioned floppy disk drive and provides a barrier to prevent scrotal skin from being sucked into the pump. The gel is used to form a seal around the base of the pump and to lubricate the penis; without it the penis will drag along the cylinder wall like an anchor on concrete.
Note to self: make sure to grab the correct white squeeze tube: the lubricating gel tube, not the menthol gel I use on sore muscles.
The caveats in the instruction manual were disturbing.
“Vacuum therapy may cause a small “blood blister” on the head of your penis. This is normal and not harmful.”
“The rings may bruise the base of your penis. Some bruising is normal and should not be cause for alarm.”
Wait, what? In what alternative universe is a bruised and blistered penis “normal?”
“If you wear a ring for more than 30 minutes, you may severely bruise or damage your penis.”
So, if that happens, do I just get a new one from Amazon with 2-day Prime delivery?
I looked over the instruction sheet I’d gotten from the P.A.
You were given samples of ED medication to try at your leisure. Please use the paper form you were given (to) track your response and side effects of each medication. The goal is for you to try one tablet every 3rd day followed by (significant) stimulation.
- Tablets work better on an empty stomach
- Tablets take one hour to become effective
- Space out your trials by 2-3 days at the minimum
If tablets do not work, you may still have intercourse with the vacuum rubber bands.
Common side effects – headache, facial flushing, nasal congestion
If you are on Cialis and are experiencing leg cramps – Please stop Cialis immediately as Cialis can sometimes be linked to tendon inflammation, possible rupture.
Oh, goody!
I discovered the vacuum doesn’t work immediately, which was disappointing. One cannot hope to instantly inflate the penis like a balloon that a clown twists into animal shapes for kids at a party. At first it took fifteen minutes to achieve anything resembling an erection, which decreased to around five minutes after three months. The least they could do is make pumps entertaining with indicator lights and an alarm that goes off when one has reached maximum height (or is it length?).
Anyone who played with a vacuum cleaner hose as a kid knows it can inflict some pain if left on a body part for too long. Moving blood into a penis with negative pressure is an uncomfortable process and certainly not erotic. And few things are worse than having a large chunk of scrotal tissue suddenly sucked into the cylinder along with a testicle. The barrier did not help at all; it was too flexible and got drawn in as well.
It didn’t take long for one of the rings to break and the replacements cost twenty bucks each. I ordered a different kind of ring that looked like a flat, silicone bagel (the penis goes through the hole and the surrounding material blocks wandering skin, but it was for a rival brand and didn’t fit my pump. I found another type that looked more like a foam-lined chip clip (or a cigar cutter). I settled on a silicone loop I bought from Amazon.
The battery pump died after a month. The company said they’d send a replacement which never arrived, and I don’t feel like calling them again. The manual pump is equally effective but using it leads to spasms in my right thumb and pain in my right wrist, caused by old nerve damage from two separate lacerations. The recommended forty-five seconds on, one minute off did nothing, even after multiple attempts over three weeks. I finally just pumped and left the vacuum on for several minutes while amusing myself with my Kindle game. (I may not have sexual function, but at least I’m doing my part to delay age-related dementia!) My erections promptly deflated as soon as I released the vacuum, despite the ring. There was never sufficient rigidity to close off the penile veins.
I then tried using 100mg sildenafil without the pump or any kind of stimulation. I got a slight flush but nothing. A few days later I made another attempt. I got distracted doing other things but applied the pump three hours after I took it. I got a reasonable erection which again deflated after taking off the pump and using the loop. I tried the pump again and then manual stimulation which made it last a little longer but still wasn’t anything to write home about. And all this took about 25 minutes, not including the minimum one hour wait for the drug to take effect.
George Burns said, ““Sex at age 90 is like trying to shoot pool with a rope.”
But all is not lost. Men can have orgasms without an erection, although it may take some mental adjustment. If you’re a New Ager into Tantra (and you have a lot of patience), you can have an orgasm using just your mind. Radical prostatectomy removes the prostate and seminal vesicles, meaning there’s no more semen, along with the sphincter between the urethra and the prostate, which normally prevents retrograde ejaculation (semen going into the bladder instead of out the penis). The result is climacturia, the release of urine with orgasm and a common side effect of the surgery. One can prevent this with an adjustable loop around the penis, muscle training or surgery, but emptying the bladder beforehand is the simplest.
More information than you ever wanted to know, eh?
Finally, nothing is more important during post-prostatectomy rehabilitation than a loving and supportive partner. Peg says she would rather have me alive and annoying than six feet under, and for that I am grateful.
Monkey illustration © Can Stock Photo / yayayoyo