I really hate what our healthcare system has become after Corporate America took over!
I had a colonoscopy in 2021 during which my gastroenterologist, Benny Thomas removed a tubular adenoma, a type of precancerous polyp, along with three other polyps. I’ve had internal hemorrhoids for as long as I can remember, so occasional rectal bleeding has never been surprising. However, over the past few weeks I’ve had much more frequent bleeding, sometimes with little clots, which would be less concerning had I not had radiation for prostate cancer nineteen months ago. Radiation treats cancer but can also trigger new cancers.
All the large health care groups where I live use MyChart®, an electronic health record (EHR), which supplanted the old paper charts. I suspect I’m not the only one who has a love-hate relationship with it. Patients can look at test results and notes from office visits, make appointments online, and, most importantly, pay their outstanding bills or copays before office visits. They can communicate easily with their health care providers or authorized designee (read: nurse) through the messaging app. Or so I assumed.
My GI guy is affiliated with Pretentious Healthcare Network (PHN), not with my usual stable of providers at the eternally aggravating Suburban Medical Group (SMG). Ruthless University Bastards (RUB) is another predatory group in the area that has an unfortunate habit of gobbling up hospitals and stripping them of “frivolous” amenities the previous owners provided to make the lives of patients and staff a little more pleasant, all in the name of “fiscal responsibility.”
I signed into PHN’s MyChart to make an appointment, but the system thought I was a new patient, because my colonoscopy was a little more than three years previously. (Three years seems to be the magic cutoff; time to cull the herd.) Nope, you’re 2 months too late; too bad, so sad. Dr. Thomas’ first available appointment was in six months, and I really didn’t want to start over with a new physician, so I called “the office.”
Now, when I was a teenager growing up in small-town Illinois, accessing health care was far less complicated. My mother would call the doctor’s office and talk with his nurse (in the 1960s most physicians were men) who would take a message, put my mother on hold, talk with the doctor, and return with instructions to come to the office or sit tight. During the night, the doctor’s wife answered the phone so he could sleep, and she would tell you to go to the ER or take two aspirin and call the office in the morning.
Not anymore, Monty. There is no way in hell I can call any office directly. Instead, there is one phone number for all the physicians in a specific practice (internal medicine, pediatrics, cardiology, etc.), or, in PHN’s case, Specialty Care, which includes a host of specialists lumped together. Physicians and nurses, people who do actual work, are shackled by the system. We are all “only pawns in game of life.” It’s another reason I’m glad I retired.
I called Specialty Care on Monday morning, and the system immediately hung up. That is probably because the people who ignored their problems over the weekend call on Monday. I thought I’d be more successful waiting until Tuesday morning after the crowd thinned out.
I connected after a couple of rings:
“Thank you for calling Pretentious Healthcare Network’s medical specialties group. If you are having a life-threatening medical emergency, please hang up and dial 9-1-1 immediately as we’re not gonna waste time resuscitating your sorry ass over the phone. Now, what do you want? Are you calling about an appointment or test results?”
Yes
“Sorry, I didn’t understand that. If you are calling to make, cancel or reschedule an appointment, say ‘appointment.’ ”
Why the fuck didn’t you say that in the first place? You asked me a yes/no question!!!
After saying “appointments” a few times and hearing “I didn’t understand that” I got connected to a live human. I explained my situation: I was an established patient; I’d had significant rectal bleeding for the past few weeks; I’ve had precancerous polyps taken out in 2021 and I had radiation in 2023. Dr. Thomas’s first available appointment on MyChart was in six months. She then asked the questions I needed to answer to continue my quest:
“What is your name?”
“What is your date of birth?”
“What is your address?”
“What is the air-speed velocity of an unladen swallow?”
Satisfied with my responses, she said she’d relay this to the doctor’s nurse who would then call me back.
I got a call three hours later from Gracie, Dr. Thomas’s nurse. I repeated my story. Did she not understand the message from the gatekeeper or is she testing me to determine if there are any discrepancies? I explained twice that I had radiation therapy which ended in March 2023.
“You need to get a CBC.”
“I had one a few weeks ago.”
“I don’t see it here.”
“You won’t because I get my bloodwork done with an outside service.”
“Do you have the results?”
“Yes, let me pull it up on my computer. Would you like me to send you a copy?”
“That would be great! Can you use the messaging app on MyChart?”
I started using an online laboratory service, DirectLabs, in 2007 when I was an independent contractor with high-deductible insurance. I ordered the tests I wanted and paid online; the company would send me a requisition approved by one of their physicians. Then I would made an appointment at any of Quest Diagnostics locations, get my blood drawn and receive my results in a day or two. It was far cheaper and more convenient than getting blood tests from one of the local providers.
I still use DirectLabs every year. I can get the Comprehensive Wellness Profile for $97; it includes:
• Comprehensive Metabolic Profile (CMP) (blood glucose, kidney and liver function tests and electrolytes)
• Complete blood count (CBC)
• Lipid profile (cholesterol and triglycerides)
• Thyroid Stimulating Hormone (TSH)
• Iron, uric acid, and phosphate
And there isn’t an additional $20 charge just for sticking a needle in my arm!
I signed into MyChart only to discover that I couldn’t send a message and attachment to her because “There are no providers you can contact.” I couldn’t reply to the last message exchange between me and Dr. because “This message is too old to respond to.” Well, fuck you very much. So, being resourceful and proactive, I printed the report and drove to the office which was only a little over seven miles away but took half an hour because the main drag was backed up like rush hour for no apparent reason.
Dr. Thomas’s office had moved to another part of the facility since my last visit. The entry from the parking lot ended at an intersection – left for the Emergency Room, right for outpatient services. I recognized the area as I’d waited here when I had cataract surgery last Halloween. My eye caught a sign for “Specialty Care Group” on the right, but it was every specialty except the one I needed. I walked farther into the area and eventually found a directory on the wall behind me.
The office was on the second floor. I got into a dimly lit elevator with three other people. The four tiny, recessed lights in the ceiling made the car feel like a sleazy city alley. I almost asked the other people if we should be afraid of being mugged but thought better of it.
I found the office and asked the receptionist if Gracie was still around (she also works in another office across town).
“Yes, but I don’t know if she’s in today.”
“I know she’s in because I just talked to her. Would you give her this?”
I handed her my report and left.
Gracie called me back while I was driving. I couldn’t answer so I waited until I got home; she left a message asking me to call her back. That meant going through the whole process yet again: waiting in the queue, “call 9-1-1, blah, blah, blah;” “appointment, dammit;” explaining to the sweet young thing; getting put on hold while she tracked down Gracie.
“I talked with Dr. Thomas. He can see you at 4:40 p.m. tomorrow but he wants you to get another CBC before he sees you.”
“Why? It’s only been a couple of weeks.”
“Have you been light-headed or dizzy?”
“No, I’m not anemic. You know I’m a physician?”
“Yeah, I kinda assumed that. But he wants another CBC.”
“Well, I’m not gonna drive back out there and waste another hour. Is there any place closer?”
“You live in Lombard? There’s one on Main Street in Lombard.”
“Is it in the sleep center?”
“No, it’s farther down, near downtown.”
(“Downtown” is a misnomer: it’s what the town used to be 100 years ago and about eight blocks long. The rest of the city is suburban sprawl.)
“Oh, I know; across from the Dairy Queen!”
“That’s it.”
The location was open until 7:30 p.m., at least according to Google. There’s an urgent care in the building and one would assume if they see patients until 7:30 p.m. that the lab would also be open should anyone need blood work. And one would be wrong.
I planned on Peg and I going there after she was finished working and before we went out to dinner. We arrived at 5:30 p.m. but the receptionist told me the lab closed at 5:00 p.m.. As we walked out, a couple in scrubs, presumably from the outpatient surgery center, said the lab closed at 4:00 p.m.. Irrelevant, since I was too late and therefore fucked.
The next morning Peg woke me up, all excited. She remembered the urgent care just up the street, a former bank, is one of PHN’s and has a drive-through lab open 6:30 a.m.- 6:30 p.m.. Technically, it’s in the next town but a lot closer than the Dairy Queen location.
It was a great setup! They had enclosed three former drive-through banking lanes with glass and aluminum garage doors. I called the number on the stop sign outside the lanes, gave someone my information, and waited for a door to open. Then I pulled in and stopped by the phlebotomist and her equipment cart. The area is climate-controlled judging by the thermostat on the wall and she wasn’t wearing a jacket (the outside temperature was about 45°). She asked me to open the door and stick my arm out. A couple of minutes later my blood had been drawn, the tube properly labeled, and I was out the door.
I went to vote early, picked up breakfast from Sonic, came home and logged on to my computer. I saw an e-mail from PHN asking me to complete online check-in to save time. It’s one of the few benefits of EHR’s. No more sitting around with a clipboard and multiple pieces of paper, trying to list your drugs on single spaced lines. I did all that and continued through email.
“There is a message from your provider’s office.” The message: “Appointment cancelled. Time: 4:20p.m..”
WTF? I called the main number and went through the queue YET AGAIN. Apparently, someone had made my appointment for 4:20p.m., cancelled it and moved it to 4:40p.m.
What might have happened if I was just a regular old person who didn’t think of pursuing this? “Well, they cancelled my appointment, so I won’t go and hope they will call me back to reschedule.”
We finally saw Dr. Thomas, a man whose rugged face and thick grey hair would make him perfect for a soap-opera physician.
“I understand you’re having rectal bleeding.”
“Yeah, it started a couple of months ago, but it’s become a lot more frequent, sometimes every day. Since I’ve had pelvic radiation, a new cancer was the first thing that popped into my head.”
“We see this a lot. You probably have AVMs – arteriovenous malformations – which are like little spider veins you see on the faces of old people. They are fragile, easily broken and likely what’s causing your bleeding. This can happen up to two years after radiation.” (I don’t remember my radiation oncologist mentioning this.)
“We can cauterize them with an APC (argon plasma coagulator) but since that requires a colonoscopy and you’ve had adenomatous polyps, we should just look at your entire colon.”
“OK, fine by me.”
He asked me to change into a gown so he could do an external anal exam, then he left the room. I could have just dropped my pants and bent over like I did during prostate exams, but whatever. When he returned he had a quick peek, which seemed hardly worth the trouble.
“It looks good. I’ll have my nurse check the schedule and find a date.”
I wasn’t prepared when his nurse returned and asked, “Would Friday (two days later) work for you?”
I had a deer-in-the-headlights moment and didn’t know what to say. Bowel preps are time-consuming and annoying. Normally one has to start with altering the diet about five days before the procedure. I reluctantly agreed, having forgotten a dinner engagement on Saturday.
Ah, but there was another fly in the ointment that would delay things. The practice puts the burden of obtaining preauthorization for procedures on the patient. Fortunately, being married to someone working for the company that provides your insurance has its benefits. Peg called and talked with the woman who was a great help when I was going to have radiation therapy in 2023.
The healthcare coding system is the bane of physicians’ existence. We need to have an International Classifications of Disease (ICD-10) diagnosis code as well as a Current Procedural Terminology (CPT) code for the procedure. There’s also the Healthcare Common Procedure Coding System (HCPCS), pronounced “Hick-Picks” that the Centers for Medicare and Medicaid Services (CMS) requires. This nonsense is yet another reason I’m happy to be out of the biz.
Our insurer doesn’t require preauthorization for a diagnostic colonoscopy, but it does for planned APC. (Pop quiz: what does APC stand for?) I returned to the phone queue, got Dr. Thomas’s nurse and went round and round over the coding, trying to get her to understand that if I didn’t get preauthorization if needed, I’d potentially be on the hook for the entire charge plus a $250 “no-no-bad-dog” penalty. The fact that MyChart prevented me from replying to her messages just added to the aggravation.
So, I took the bull by the short ones and searched Google. I found the “2023 Coding & Payment Quick Reference” put out by Boston Scientific which had a code for “Colonoscopy, flexible; with control of bleeding, any method,” and sent it back to the nurse. The next morning, I was roused from my slumber at 8:00 am (no, I am NOT a morning person!). The doctor was happy with using that code and so was the preauthorization person. He also had a cancellation for the following Thursday, which worked out for us.
I ran into a minor snafu at the pharmacy with the bowel prep. The main ingredient in all bowel preps is polyethylene glycol (PEG-3350), the stuff in Miralax. Industrial-strength preps like Nu-Lytely (Gavalax-N is the generic), add sodium and potassium chloride, and sodium bicarbonate to minimize the electrolyte loss and potential cardiac complications of flushing one’s bowel with a gallon of fluid.
However, the most reviled of modern bowel preps is Go-Lytely, an evil concoction with sodium sulfite added to the other electrolytes. The result is something that smells and tastes like rotten eggs and is very salty. It’s one of the reasons most people hate bowel preps. The pharmacy wanted to give me Go-Lytely, but it appeared that Nu-Lytely had also been prescribed, so I took the latter.
The prep went relatively well, although chugging down half a gallon of cold solution that tastes like flat lemon-lime soda in less than three hours is a challenge. It might have been easier if the outside temperature was in the 90s instead of mid 40s. I warmed up some apple juice with a cinnamon stick to ward off the chills.
The Endoscopy Center called me mid-afternoon to tell me my procedure would be at 1:15 p.m.. I had to drink the other half gallon of solution starting six hours before getting the tube, so at least I could sleep all night. Squirting warm, yellow liquid out your butt isn’t pleasant, but it could be so much worse.
We got to the Endoscopy Center a little before noon. I had my driver’s license, my Medicare card, and my insurance card in hand, but all the receptionist wanted to know was my birth date and home address. The waiting area was in the hall and seating was limited; we ended up in a couple of chairs just outside the double doors leading back to the suites.
About twenty minutes later a nurse in scrubs came through the door and said, “Harold.” A woman next to her yelled, “Hank! HANK! Get back here; they’re calling you.” Hank had gotten a little bored and wandered down the hall for no apparent reason, much to his wife’s irritation. I heard her say to the nurse, “Tell him he can’t go roller skating tonight!” (My postoperative instructions cautioned against making critical decisions and operating any kind of machinery, “including kitchen appliances.”)
My turn came sooner than I expected, but was still a lot later than it should have been. A sweet young nurse named Cassidy, probably shy of thirty years, ushered us into the same room Peg had occupied when she had her colonoscopy, sans sedation, several years ago. I knew the drill very well: strip completely, put on the patient gown, open to the back, get on the cart and wait for her to put on EKG leads, take my blood pressure and pulse oximetry, and then start an IV.
Sometime during all this Peg mentioned I was a physician (after thinking Cassidy was talking to me like a five-year-old), and she perked up.
“What kind of physician?”
“Obstetrics.”
“I was an obstetric nurse at Holy Smokes Hospital!”
“How long ago?”
“About four years”
“I worked there in 2010.”
“I graduated high school in 2014!”
OK, so I could be either your father or grandfather. Thanks a lot.
Several minutes later Cassidy returned to tell us things were running late. Dr. Thomas was finishing one procedure; he had another, shorter procedure, before it was my turn. She left and I closed my eyes to ward off the boredom.
Then I heard a procession in the hall with someone yelling, “Frank. FRANK! We’re done and we’re going back to your room. Stop trying to get off the cart!” (Frank growled something unintelligible, which faded as they passed).
Finally, I saw Dr. Thomas, who asked us if we had any questions, followed by the CRNA who went over my medical history. Peg and I both stressed that I had a paradoxical reaction to benzodiazepines like Versed, which, along with fentanyl, is often used for sedation. She assured us they only used propofol. A few minutes later one of the OR nurses came to take me to the room.
“Wait a sec. I should go to the bathroom one last time.”
“Number one or number two”?
“Number one…what?” (Do I look like I’m a fucking kindergartener???)
“If it’s number two, don’t worry. We suck everything out anyway.” (I’ll keep that in mind for next time.)
I went into the restroom just across the hall and then climbed back onto the cart before she wheeled me into the procedure room.
Now, I’ve mentioned before how I find anesthesia fascinating. The conscious brain is disconnected from the rest of the brain and body, and it feels like time stops. This time I remember the dark curtain falling as they pushed the propofol. Hasta la vista; meet you on the other side.
IV sedation also removes inhibitions until the consciousness fully recovers. Apparently, I was a potty mouth when I returned. It started when the nurse was trying to adjust my blood pressure cuff and get me off my left side, where I’d been lying since the procedure began. Peg relayed my comments after I’d regained some semblance of coherence:
“This is bullshit! Pardon my French.”
“They fucking zapped my ass.”
“That guy on the cart who tried to do a runner was an asshole.”
“Propofol is fucking great!”
I felt bad for exposing Cassidy to such profanity, but Peg assured me I was probably the least of her problems. An able-bodied man in the next room, waiting for his wife to return, was too fucking lazy to go to the bathroom across the hall and instead, peed into a urinal he found in the room. The problem was his aim sucked, and the poor nurse was left to wipe his pee off the floor, then empty the urinal in the bathroom because he was too lazy to do it himself.
I still think I should send Cassidy a note with an apology.
As suspected Dr. Thomas found several arteriovenous malformations, the source of my bleeding. Here are before and after pictures.
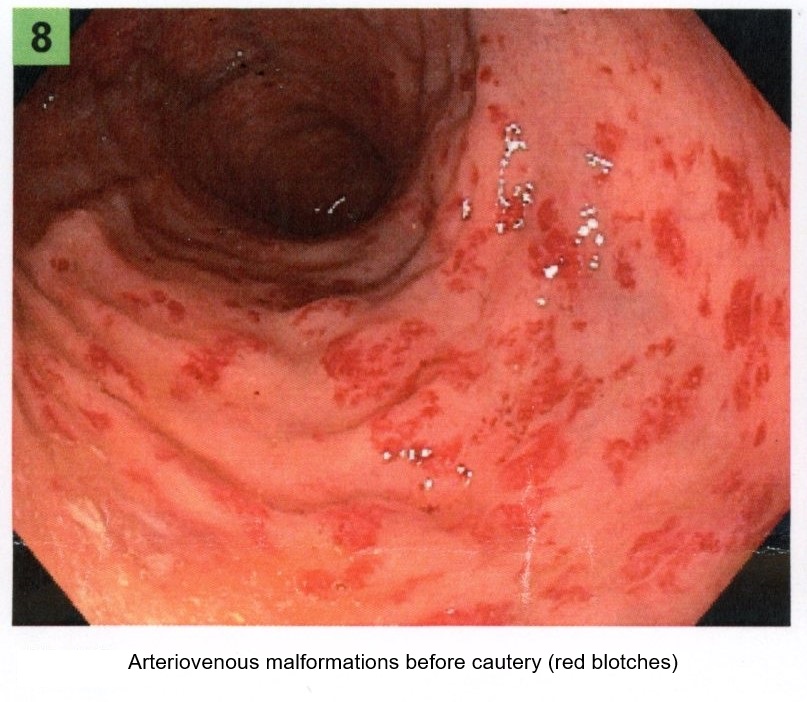
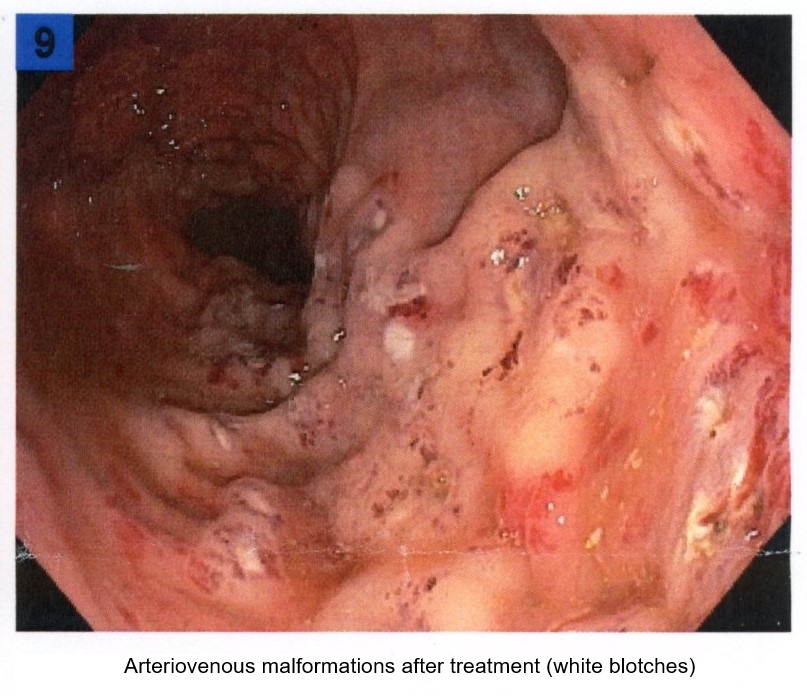
He also snagged four pre-cancerous tubular adenomas. I think I’m predisposed to other cancers, given I’ve already had prostate cancer and pelvic radiation. So now I’m on the three-year plan. I’ve already set a notification to call the GI office before the end of three years, so I don’t have to repeat this bullshit.
I had a phone visit with my radiation oncologist two months later.
“You should really tell your patients about arteriovenous malformations.”
He paused for a moment.
“I developed rectal bleeding and…”
“Oh, I thought you were talking about brain AVM. Yes, this is radiation proctitis and it happens in about 1% of patients.”
(Yeah, well that would have been nice to know).
It’s been seven months, and I haven’t had any more bleeding. But my PSAs are still rising, so I’ll be seeing the radiation oncologist again next month. Good times.
